Comments
- No comments found
Covid-19 was a dry run . . . It was kind of a fire drill for what has yet to come, and the truth is we still aren’t ready.
I vividly recall sitting and testifying in front of members of the US Congress and Senate sometime in 2013. Their questions were well-thought-out and prepared. They were doing their due diligence as members of the elected public trust to make sure we were prepared for the health care disaster they predicted might befall us.
That naturally being . . . What should we do to prepare for an earthquake striking the Midwest?
Yeah . . . you heard me right . . . their biggest mass casualty fear was an earthquake striking the Midwest.
Then Congressional representatives Susan Brooks, Todd Young, and Jackie Walorski and Senator Joe Donnelly sat across from us as a few other physicians from other local medical centers weighed in. I listened as my colleagues from other institutions puffed out their chest for the representatives and the cameras and touted their capabilities or operating capacity, or an ability to deploy a MASH-type army tent in the middle of a parking lot with some fold-out cots (a visual that wooed the hopelessly naive). Then they got to me and—well . . . never being once to mince words—my response went something like this:
“Why are you worrying about an earthquake? We aren’t even prepared for a flu pandemic.”
Nobody really listened, or if they did they just politely nodded their heads. Don’t believe me? Look it up.
But in all transparency, during that time, I wasn't really contemplating Covid-19. I was thinking about a strain of Spanish flu similar to what killed tens of millions of people during the turn-of- the-century. You know, during a time when we had a fraction of the number of people on this earth and we weren’t able to literally traverse the globe in a matter of hours shedding infection from one major population center to another. I had already seen the impact of H1N1 and had been in medical school during HIV, and at that time of my life I was tasked with mass casualty preparedness for our group So I had been thinking about it for a while. Most ER docs had.
Now it’s time for the polite head-nods to end and for those in charge to really listen and review what we have learned and what we have ignored and steps we need to take. So, here’s some starting points and observations from someone who has been in this shit from day one.
First off, it didn’t kill children. It also didn’t kill your average healthy person. Why does this matter? Because the first group is the heartbeat of our country. The second group is the cog in the engine that keeps this country running. I want you to stand back for a second and think about what this country would look like right now if mortality was evenly distributed across the age groups. We have had nearly 850,000 US deaths from Covid-19 and 74% of those were over the age of 65 with 95% being over the age of 45. There have only been about 900 children under the age of 18 that have died of Covid-19 and many of those had significant co-morbidiries. It seems like a lot, but in the grander scheme influenza and RSV kills about the same number of children each year and those illnesses result in far more hospitalizations in children than Covid-19. If children had been dying at their representative rate within the US population, we would have had something like 150,000–170,000 deaths in children and probably a million hospitalized. Can you imagine how this would have led to an absolute collapse of society? Do you honestly think health care workers, especially those with children, would have shown up if they had any inkling that they could bring that kind of viral pathogen into their home?
We are not prepared for THAT prospect and we have to have that taskforce discussion now. Because those healthcare heroes that you so readily touted, me included, will probably stay home if the next pandemic has that degree and demographic distribution of pathogenicity. Like it or not, our families are just as important as your family.
So then, why did we, the health care workers, show up this time? Well you have to realize, in the early days of this pandemic we were primarily looking at Italy way before Covid-19 hit our shores. We sure as hell weren’t getting what we needed in terms of on-the-ground bedside data from China (which is all you need to know about their level of cooperation). We were waiting first and foremost to see if people, like us, were dying in Tuscany hospitals. We were, at times, watching the WHO and CDC websites, but we knew the real skinny was happening at the bedside in Florence, not in the war room of the CDC.
We were glued to our physicians and nurse social media platforms that were in close touch with our colleagues in Venice and Rome, who were also posting on our same message boards. We weren’t taking our cues from some government or internationally-run agencies who usually were weeks behind us. All we cared about was what the ER and ICU docs on the ground in the trenches in Italy were seeing. We knew early on they weren’t seeing young, healthy people dying, and that their docs and nurses were for the most part doing OK.
So we came to work, masked up, gowned up, put on shields, and hunkered down for the onslaught of death headed our way, but we kept a real close eye on our colleagues at the computer next to us, seeing if they would start falling—and since they weren’t dying with any regularity, we carried on. In torturous conditions, we continued to show up. If that had not been the case, our ER Facebook groups would have been flooded with messages on the best place to buy pallets of peanut butter, water purifiers, generators, and canned beans. Instead of posting questions like What’s the best way to prone a patient to oxygenate the posterior lung fields? Does dexamethasone really work? Can you ventilate two patients with one machine?, and on and on. It’s as simple as that. We weighed the risk in real time, it didn’t seem so risky as long as we were careful. It took months for the CDC to catch up with what we already knew. The ability to crowdsource knowledge in real time with real doctors at the bedside was beyond valuable.
The CDC missed a huge opportunity to partner with groups like EM DOCS on Facebook and countless others to spread their message and to have open and honest real-time dialogue with those at the bedside. Give me 22,000 bedside docs any day over a government-appointed shaman with an MD. My colleagues saved America along with the scientists who developed the vaccines—and my colleagues were the MDs, the DOs, the nurses, the PAs, the therapists, the techs, the housekeepers, and countless others who were at the bedside. Next pandemic, they need to run the show.
As I said in the article in 2014, we have to protect medical centers from the flu. Covid-19 essentially destroyed our ability to provide day-to-day medical care, elective surgeries, cancer screening, and more. Thousands have and will die because of this failure. Those numbers are hard to figure, but they deserve close scrutiny. We have to reinvent our ICUs and our provision of palliative care and build massive open-ward, bare-bone, viral hospitals offsite from the main hospital. This will also require a comprehensive agreement on who will and will not be put on a ventilator.
One of the things we learned early on was that nearly every elderly person, especially those over the age of 85 put on a ventilator for Covid-19 died. Which means we have to have concrete guidelines that move these people directly to palliative care. We simply can’t tie up all the ICU space and ventilators for people who have almost zero chance of surviving. These are hard and difficult truths we were not prepared to address, and we certainly were not prepared to deal with family members who could not come and visit their elderly parents and grandparents as they died or were holed up in extended care facilities. There is no reason that in the twenty-first century we cannot have the infrastructure in place to make this happen, even in the middle of a pandemic. We as doctors and nurses should not have to stand with a phone and FaceTime sons and daughters so they can watch their moms and dads die. That’s not a compassionate death. This will haunt many of us for years to come. It created an incredible amount of emotional stress on doctors and nurses and the families of those dying. Covid-19 took compassion out of dying. We are a better country than this.
This was not so much a policy issue, though some unyielding concrete thinkers in administration made it so, as it was an infrastructure issue. The ICUs are not built in a way that family members can visit during a pandemic, even if it’s just on the other side of a glass partition. ICU wards today are simply not designed to manage any pandemic or even a mass casualty event. This physical plant idiocy can be traced way back to HIV and HIPPA privacy issues where we became obsessed that the person in the next bed might know we were on Zoloft, or had our gallbladder removed in ’92, or crapped blood in ’87. This has to end. ICUs and even some ERs need to be open, contained-airflow wards with lines of beds where nurses and techs and respiratory therapists can move freely from bed to bed. Where the ventilators and all tubings come through a walled partition and are managed outside the contagion confines. There is no reason a nurse should be regowning and masking and going in and out of the same room dozens of times a day when the bulk of their care can be managed without exposing themselves to pathogens. In addition it is beyond exhausting to work like this. Put 20 ICU docs, 20 ICU nurses, 20 respiratory therapists, 20 radiology techs, and 20 housekeepers in a room and in a week you will have the design for a state-of-the-art ICU that can be replicated in any state in America. This is a civil defense initiative that has to begin now. States should not wait for the Feds to do this. Be creative—combine resources but get it done now.
Let’s review. We rapidly developed, in record time, a novel vaccine that had a very high efficacy in preventing deaths. Not in stopping transmission . . . in preventing deaths and that’s all that matters. This fundamental truth, due to shitty messaging by those in Washington, was lost on a huge portion of the population and was and is an abysmal failure of leadership. It created division, and skepticism and resulted in tens of thousands of deaths by those who went unvaccinated. The end game has always been about preventing death and disability, not transmission, and not preventing millions from pronouncing that “I tested positive or got sick with a fever and body aches.” Plenty of people got vaccinated and still got Covid . . . so what. But pretty much all who died of Covid and still are dying of Covid are unvaccinated. That’s all that matters. The vaccine kept you alive.
This vaccine was a medical marvel, the equivalent of knocking a meteor out of an impending collision with the earth by firing a mortar out the back window of the space station—and we ramped up its production way before it was even approved, guaranteeing that hundreds of thousands of lives were saved. This was a success. Once the political posturing fades, hopefully this will be celebrated in epic ballads for years to come and extrapolated to other pathogens in the future. Because, right now, the efficacy of flu vaccines does not come close to approaching this rate of success we have seen with Covid-19 vaccines. We have to pour billions into this and make this happen for the flu. The structure of the flu virus is a whole new animal. In a lot of ways it’s even scarier because of the rate it rearranges its coat structure. We know the gene sequences of the nuraminidase and hyaluronidase proteins from the Spanish flu and some of the other proteins from that virus. There are also some theories that co-pathogens might have played a role in its virulence in the turn-of-the-century. What we need to know is, can mRNA technology be used to replicate this process in influenza—and if so should we be stockpiling doses and monoclonals targeting key influenza proteins in addition to antivirals and other therapeutics? It’s not enough to have a model in theory; we have to have it ready to go and administered in weeks. That infrastructure is not in place, and it has to be considered as a form of national civilian defense and they have to be manufactured on our shores.
This is just a peek at a few of the things I hope to bring to light in the aftermath. I’ll get to nursing shortages, and administrator failures in latter segments. I’m just getting warmed up and hoping that perhaps someone is listening. I'm getting old for an ER doc. I know I will most likely not be practicing the next go-around. I’ll fade away in a few years, but the risk to my family, to my community, and to the people I love will remain. Covid-19 has exposed some major gaps and inefficiencies in how we provide care during a pandemic. One of the things history has taught us from the Holocaust to 9/11 is that we have a very short memory when it comes to the dangers and evils that can befall us. If you, the decision makers, don’t listen to the people who were at the bedside for the last two years, you are doomed to repeat these mistakes but on a grander scale in round two . . . and trust me when I say . . .we won’t forget it.
Dr. Louis M. Profeta is an emergency physician practicing in Indianapolis and a member of the Indianapolis Forensic Services Board. He is a national award-winning writer, public speaker and one of LinkedIn's Top Voices and the author of the critically acclaimed book, The Patient in Room Nine Says He's God. Feedback at louermd@att.net is welcomed. For other publications and for speaking dates, go to louisprofeta.com. For college speaking inquiries, contact bookings@greekuniversity.org.
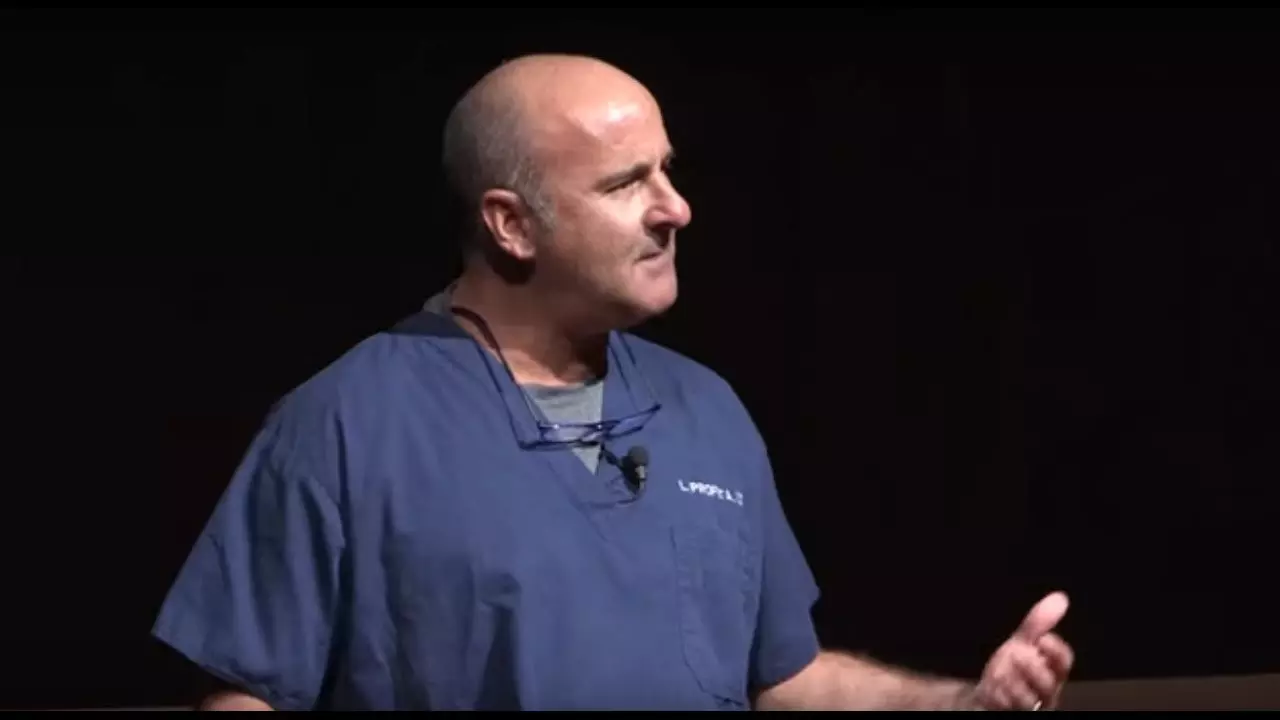
Dr Louis M. Profeta is an emergency physician practicing in Indianapolis. He is one of LinkedIn's Top Voices and the author of the critically acclaimed book, The Patient in Room Nine Says He's God. Dr Louis holds a medical degree from the Indiana University Bloomington.
Leave your comments
Post comment as a guest